Medicaid Pediatric Recovery Program
In 2020, EOHHS, implemented the Pediatric Primary Care Relief Program and the Pediatric Primary Care Rate Supplement to support system resiliency, improve immunization rates, and overcome COVID-19 related barrier to access.
In 2022, disruptions caused by COVID-19 continued to persist and create barriers to essential preventive healthcare services. Therefore, the Medicaid Pediatric Healthcare Recovery Program provided another round of payments to pediatric and family medicine practices. Payments were contingent on practices meeting well-child visit targets or demonstrating 5% improvement over four months (March – July, 2022). In addition, practices participated in learning sessions related to developmental, psychosocial, and behavioral health screening.
Well Child Visit Performance
100% of the practices enrolled in the program, met the April and July targets or improvement targets, resulting in thirty-eight thousand Medicaid children (primary coverage) receiving well child visits from July 1, 2021 – June 30, 2022. Total payout to practices was $6.0 million.
|
3-11 year olds Rate |
12-17 year olds Rate |
Overall Composite Rate |
|
|
March submission - Baseline (1/1/21-12/31/21) |
78.1% |
75.0% |
76.9% |
|
April submission (4/1/2021-3/31/2022) |
78.4% |
75.5% |
77.3% |
|
July submission (7/1/2021-6/30/2022) |
80.2% |
77.3% |
79.1% |
Behavioral Health Learning Sessions
100% of the practices enrolled in the program participated in the behavioral health learning sessions and 11 practices took advantage of the free practice specific behavioral health technical assistance. Total payout to practices was $1.3 million. A huge thank you to Liz Cantor and Sarah Hagin for leading this effort.
- 217 people attended the behavioral health learning sessions
- Looking at the evaluation results
- 100% said that the materials presented met the stated objective
- 98.1% overall opinion of the sessions was good (17.5%) to excellent (80.6%).
- 95.6% thought the content was just right (other choices were too advanced or too basic).
- “I will be able to use the content of this session in my practice” 48.1% strongly agree; 45.0% agree with that statement
- 46.9% (75 individuals) suggested that they are interested in customized Psychosocial / Behavioral Health technical assistance.
- 75% are interested in CME credit for the sessions
- Recordings, presentations and evaluation forms can be found here.
Practice Facilitation support
In addition, practices received Practice Facilitation support, which consisted of focused discussions on well-child visits, measurement specifications, Immunization (including COVID) and Lead Screening results, as well as needs around behavioral health. A huge thank you to the practice facilitators, Vicki Crowningshield, Susan Dettling, Suzanne Herzberg, and Kim Nguyen-Leite for assisting practices in any way needed.
KIDSNET Immunization and Lead Screening Support
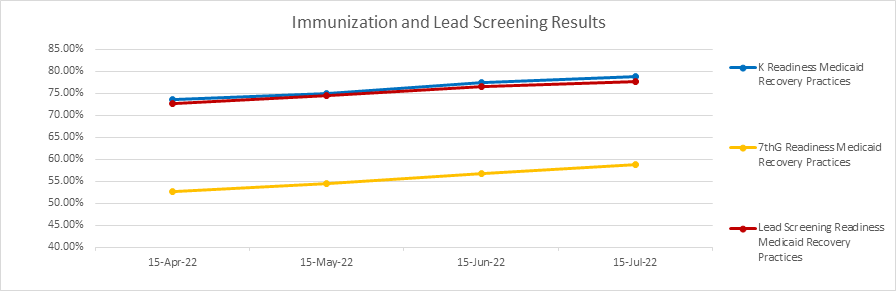
RIDOH’s KIDSNET’s assistance with providing Immunization and Lead Screening results monthly, consulting at numerous meetings and providing direct support to practices was greatly appreciated. A special thanks to Ellen Amore and Janet Limoges. As a group, childhood immunizations (including lead screenings) have improved across all categories. See graph below for performance overtime.
We want to provide a special shout out to Amy Katzen, Director of Policy and Strategy, RI EOHHS and Kim Pelland, Health System Transformation Director RI EOHHS for their leadership and hard work with operationalizing the application and payment process, done in record speed. This project resulted in $7.3 million paid to pediatric practices.
Funding for this program was provided by EOHHS and the Medicaid Pediatric Healthcare Recovery Program.
Our Mission
The mission of CTC-RI is to support the continuing transformation of primary care in Rhode Island as the foundation of an ever-improving integrated, accessible, affordable, and equitable health care system. CTC-RI brings together critical stakeholders to implement, evaluate and spread effective multi-payer models to deliver, pay for and sustain high-quality, comprehensive, accountable primary care.
