Rhode Island Ranks 4th in the Nation for State Health System Performance
Commonwealth Fund 2025 Scorecard Reaffirms State’s Strong Standing for Third Year in a Row
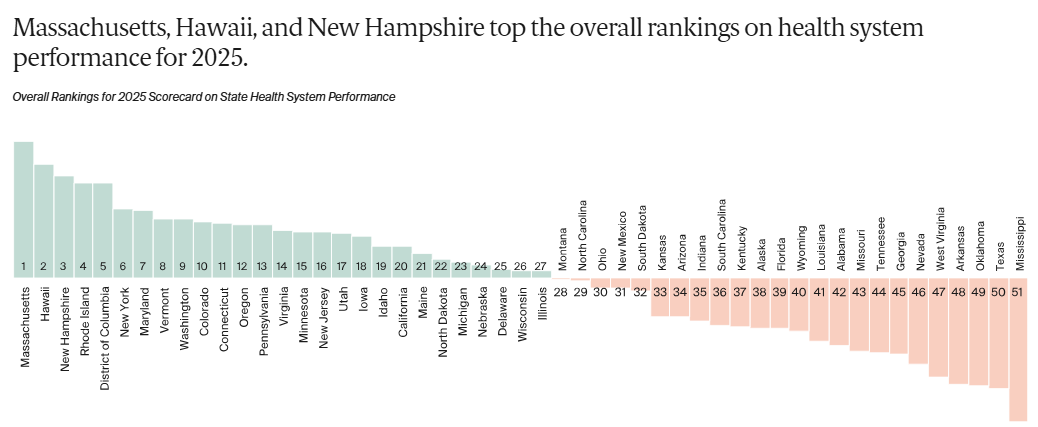
Rhode Island has once again ranked 4th in the nation in the Commonwealth Fund’s 2025 Scorecard on State Health System Performance, maintaining its top-tier position from 2024 and 2023. This sustained national recognition reflects Rhode Island’s commitment to building a high-quality, accessible, and equitable health care system, while also acknowledging that work remains to ensure every community benefits equally.
- Full Report: 2025 Scorecard on State Health System Performance
- Rhode Island Performance Snapshot (PDF)
- Appendices – Rhode Island Data
According to the report:"Topping the 2025 Scorecard’s overall health system rankings are Massachusetts, Hawaii, New Hampshire, Rhode Island, and the District of Columbia, based on 50 measures of health care access and affordability, prevention and treatment, avoidable hospital use and costs, health outcomes and healthy behaviors, income disparity, and equity."
The report also emphasizes that high-performing states often share key strategies: expanded eligibility for public insurance programs, targeted investments in primary care and behavioral health, and focused initiatives to reduce health disparities.
Rhode Island’s Standout Performance
- Overall Ranking: Rhode Island is ranked in the top tier nationwide, joining Massachusetts, Hawaii, New Hampshire, and the District of Columbia as high performers in health system effectiveness.
- Access and Affordability: The state excels in ensuring its residents have access to care, with one of the nation’s lowest uninsured rates and the lowest out-of-pocket medical spending, contributing to a more affordable health care environment.
- Prevention and Treatment: Rhode Island continues to show leadership in preventive care, clinical treatment quality, and equitable outcomes across populations, benefiting from its well-coordinated health initiatives and strong public–private partnerships.
Beyond the Numbers: Challenges on the Ground
At the same time, rankings alone do not fully capture the realities facing Rhode Island’s health care system. Like many states, Rhode Island continues to struggle with persistent challenges, including workforce shortages, financial pressures in primary care, fragmented care delivery and healthcare disparities, and the difficulty of connecting across silos in a complex system.
Despite its strong performance, Rhode Island is not immune to the pressures facing health care nationwide. Workforce shortages across primary care and behavioral health, rising costs, and growing demands for integrated services strain providers’ ability to deliver care. Payment reform and system-level coordination are ongoing areas of development within the health system. These realities underscore that health system transformation extends beyond data to encompass building connections across silos, sustaining the workforce, and fostering an environment in which providers can thrive in caring for their patients.
Turning Data into Action: CTC-RI’s Role
At CTC-RI, we recognize the importance of celebrating progress while directly addressing challenges. Many of the issues highlighted in state and national reports are already being tackled through collaborative work with providers, health plans, community partners, and state agencies, including:
- Strengthening the primary care workforce through recruitment, retention, and advocacy support.
- Optimizing team-based care and integrating behavioral health services across the lifespan.
- Enhancing care coordination and patient access via nurse care management and community health workers.
- Using data to close gaps in care, reduce disparities, and improve chronic disease outcomes.
- Piloting innovations such as pharmacy integration, remote patient monitoring, and specialist collaboration in primary care settings.
- Advancing payment reforms to create financial stability for primary care practices.
Continuing the Momentum
Rhode Island’s consistent top-five national ranking reflects years of collective effort. But maintaining this position, and ensuring it translates into lived improvements for patients, requires ongoing investment and collaboration.
At CTC-RI, we believe transformation happens at the intersection of data, equity, and real-world practice change. By convening diverse stakeholders and piloting innovative solutions, Rhode Island can continue to be a national model for high-quality, affordable, and inclusive care.
Spotlight: Commonwealth Fund Perspective:
We invited David Radley, PhD, MPH, senior scientist at the Commonwealth Fund and lead author of the Scorecard, to provide his perspective on what these findings mean for our state, lessons that can be applied nationally, and how we can prepare for the challenges ahead.
 Q1: What does the 2025 Scorecard mean for Rhode Island, and how can we use this information to progress patient care and outcomes?
Q1: What does the 2025 Scorecard mean for Rhode Island, and how can we use this information to progress patient care and outcomes?
Our Scorecards offer a comprehensive look at how well the health care system is working for Rhode Islanders—looking at things like access to care, the quality of care people receive, and the health outcomes people in the state experience.
Rhode Island ranks 4th overall, with strong performance on measures of access, health outcomes, and health equity. But the report also points to areas where Rhode Island has room to improve. In particular, there were several care quality and cost metrics where Rhode Island performed well below the national average, suggesting that targeted interventions may lead to improved care for patients.
Q2: Rhode Island remains in the Top 4 states for overall health system ranking. What can other states learn from our progress?
Rhode Island has consistently received high marks in our Scorecards, even going back to our first state report nearly two decades ago. One of the areas where Rhode Island has stood out is on measures of access to care.
In the most recent data, about 6% of working age adults in the state were uninsured, that’s about half of the national average. Part of the reason Rhode Island has a low uninsured rate is that is was among the first states to expand its Medicaid eligibility requirements under the Affordable Care Act—making coverage available to more lower-income people in the state. However, those coverage gains are at risk; the Urban Institute estimates that as many as 32,000 Rhode Islanders could lose coverage as a result of recent federal policy changes.
Q3: Up against primary care workforce shortages, on top of federal policy changes and funding cuts—how can Rhode Island address and prepare for future health challenges?
Rhode Island isn’t alone in the challenges facing its health system. While there isn’t a one-size-fits-all approach for strengthening the system, there are things states can do. For example: endeavor to implement new federal Medicaid work requirements in ways that align with state-values; work with employers in the state keep premiums and cost-sharing in private plans affordable for employees; strengthen primary care with training support programs and licensing requirements that allow people to practice at the top of their training; and uncouple health care spending from the volume of services provided, linking payment to health care quality.
CTC-RI extends our sincere thanks to David Radley and the Commonwealth Fund team for sharing their insights and for their ongoing work to track and advance state health system performance nationwide.
