What is CTC-RI?
Mission
The mission of CTC-RI is to support the continuing transformation of primary care in Rhode Island as the foundation of an ever-improving integrated, accessible, affordable, and equitable health care system. CTC-RI brings together critical stakeholders to implement, evaluate and spread effective multi-payer models to deliver, pay for and sustain high-quality, comprehensive, accountable primary care.
Vision
Rhode Island has a thriving primary care system that ensures every person has equitable and affordable access, engages patients and families as active partners, and results in excellent health for patients, families, and communities.
History
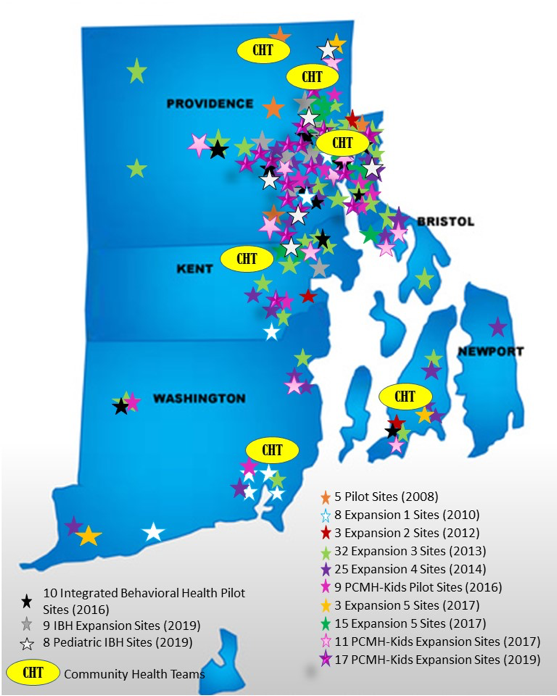
 Convened in 2008 by the Office of the Health Insurance Commissioner (OHIC) and the Executive Office of Health and Human Services (EOHHS), CTC-RI began with five pilot sites and has grown to 128 primary care practice sites, including internal medicine, family medicine, with pediatric practices (PCMH-Kids) being added in 2016. Currently, over 700,000 Rhode Islanders receive their care from CTC-RI and PCMH-Kids practices.
Convened in 2008 by the Office of the Health Insurance Commissioner (OHIC) and the Executive Office of Health and Human Services (EOHHS), CTC-RI began with five pilot sites and has grown to 128 primary care practice sites, including internal medicine, family medicine, with pediatric practices (PCMH-Kids) being added in 2016. Currently, over 700,000 Rhode Islanders receive their care from CTC-RI and PCMH-Kids practices.
In 2015, CTC-RI incorporated as a 501c3, establishing a Board of Directors as its governing body. CTC-RI is supported by funding from public and private payers in Rhode Island, along with grant funding from government and non-governmental sources.
The health plans also provide direct support for the practices through the Common Contract, an agreement negotiated between the health plans and the participating practices under the auspices of OHIC and EOHHS. The contract calls for supplemental per member per month payments designed to drive and support practice transformation, team-based care and quality improvement. These payments allow the practices to make patient-centered enhancements to successfully apply for national PCMH recognition, hire onsite care management/coordination to impact at-risk patients and families, and enhance data capabilities to manage and improve population health.
Effect
PCMHs improve health outcomes, help patients have better care experiences and reduce expensive, unnecessary hospital and emergency department visits. Here in Rhode Island, CTC-RI practices are showing that effective PCMHs truly make a difference for patients, families, providers and payers, and contributes to overall health care system improvement.
Utilization
Since 2012, CTC-RI has tracked the number of inpatient hospitalizations, organized in 5 Adult cohorts. Compared with non-patient-centered medical home practices, all 4 cohorts have greater reduction rates of patient hospital admissions, compared to the comparison group; Cohort 1 PCMH Kids practices have shown a 2.5% reduction in Emergency Department utilization compared with comparison group.
Clinical Quality
Performance incentives on clinical quality measures related to diabetes, depression screening and follow-up, colorectal cancer screening, tobacco cessation and hypertension in adults and developmental screening, obesity screening and counseling, in children, and well-child visits for adolescents have proven to drive population health improvements in CTC-RI and PCMH-Kids practices. Practices have met initiative-wide benchmarks set for each measure and/or made significant improvement over their baseline results.
Patient Experience
According to 2017 Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey, patients are realizing the immediate benefits of CTC-RI. CTC-RI and PCMH-Kids practices, as a whole have demonstrated directional improvement for access, communication and office staff.
Enhanced Learning and Services
Integrated Behavioral Health
In 2016, 10 Adult CTC-RI internal and family medicine practices began pilot-testing the onsite integration of behavioral health providers. The aim for the pilot project was to establish a sustainable financial model for integrated behavioral health and test a clinical model of increased screening for behavioral health disorders, intervention at the primary care site for mild to moderate conditions, and increased collaboration with specialty behavioral health providers. Additionally, in 2016 PCMH-Kids practices participated in behavioral health learning collaboratives by taking a deep dive into ADHD and the intersection of primary care, pharmacy, schools, and communities. In 2017, PCMH-Kids behavioral health learning focused on postpartum depression screening. Currently, PCMH-Kids practices are participating in a behavioral health learning collaborative to learn best practices for Screening, Brief Intervention, and Referral to Treatment (SBIRT) for the adolescent population. Practices incorporate practice-based quality improvement strategies to increase youth substance use screening, support youth in refraining from substance use, motivate youth to decrease substance use and identify and refer youth at highest risk.
Community Health Teams
While the focus of this initiative is on the transformation of primary care, CTC-RI recognizes that 80% of our health is determined outside the walls of the primary care office. Therefore, in 2014, CTC-RI piloted two CHTs comprised of community health workers and behavioral health clinicians that serve as an extension of the primary care team to address the social, behavioral, and environmental needs of patients with complex needs. CHTs are able to improve patient care, heath, and quality of life, while reducing cost/unnecessary utilization. Additional CHTs have since been funded, and a specialty substance use screener has been added to all teams.
Advancing Value-Based Primary Care
CTC-RI convenes regularly occurring forums for practices to stay engaged after completing the Common Contract. Quarterly Breakfast of Champions, our Annual Conference and “best practice” meetings bring together the primary care community and systems of care to share innovations tested in the multi-payer value-based environment.
Looking Forward
 CTC-RI and PCMH-Kids will continue to provide an important voice for primary care. Our multi-payer table is uniquely situated to bring together key stakeholders who will select, test and evaluate innovative clinical strategies to build the capacity of the primary care team to meet the needs of children, adults and families living in our communities. Such work is intended to result in better care, smarter spending and informed public policy.
CTC-RI and PCMH-Kids will continue to provide an important voice for primary care. Our multi-payer table is uniquely situated to bring together key stakeholders who will select, test and evaluate innovative clinical strategies to build the capacity of the primary care team to meet the needs of children, adults and families living in our communities. Such work is intended to result in better care, smarter spending and informed public policy.
The Care Transformation Collaborative of Rhode Island has a growing impact across the state, and includes:
- 190 primary practices, including internal medicine, family medicine, pediatric practices; 27 primary care practices are a part of the integrated behavioral health initiative.
- Over 900,000 Rhode Islanders receive their care from one of our practices.
- 850 providers across our adult and pediatric practices.
- Investment from every health insurance plan in Rhode Island , including private and public plans.
- All Federally-Qualified Health Centers in Rhode Island participate in our Collaborative.
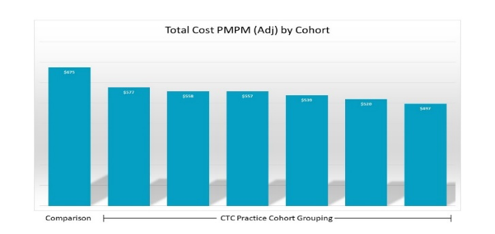
- CTC-RI practices demonstrate lower total cost of care by $217 million in 2016 when compared to non-patient-centered medical homes in Rhode Island, according to data from the state’s All-Payer Claims Database.
Practices
See a list of current CTC-RI practices here.
See a list of graduated CTC-RI practices here.
Get Involved
Are you interested in becoming a patient-centered medical home? Have you achieved medical home recognition but are looking to further transform your practice? Contact us at CTC-RI@ctc-ri.org.
CTC-RI Nurse Care Manager / Care Coordinator Opportunity to Apply for GLearn Core Curriculum Training Program
Our Mission
The mission of CTC-RI is to support the continuing transformation of primary care in Rhode Island as the foundation of an ever-improving integrated, accessible, affordable, and equitable health care system. CTC-RI brings together critical stakeholders to implement, evaluate and spread effective multi-payer models to deliver, pay for and sustain high-quality, comprehensive, accountable primary care.
