Overview and Results of CTC IBH Adult Pilot Program
Integrated Behavioral Health Pilot Program Funders
 |
 |
 |
Overview
It is widely recognized that unaddressed Behavioral Health (BH) conditions increase suffering and total cost of care and that BH drives 60-80% of all visits to Primary Care (PC). Building and supporting the delivery of integrated behavioral health care at PCP sites is fundamental and necessary to improve quality of life and to decrease inefficient utilization of health care services and dollars.
The Care Transformation Collaborative of Rhode Island (CTC-RI) was awarded grant funding through the Rhode Island Foundation's Fund for a Healthy Rhode Island to test a clinical and financial integrated behavioral health (IBH) proposal. CTC-RI issued a "call for applications" in October 2015, and twelve CTC-RI Primary Care Practices were selected to participate in either Cohort 1 (January 2016 start date) or Cohort 2 (November 2016 start date) for a three year IBH Pilot Program. Ten practices completed the program.
The objectives were to: 1) increase the identification of patients with behavioral health and substance use disorders (SUD) through universal screening for depression, anxiety and SUD; 2) increase ready access to brief behavioral health intervention for patients with moderate depression, anxiety, SUD and co-occurring chronic conditions; 3) provide care coordination and intervention for patients with high emergency department (ED) utilization; 4) improve interdisciplinary care coordination for patients with severe mental illness and SUD; and 5) test the proposed financial model for long term sustainability with particular attention to ED and inpatient (IP) utilization/total cost of care as sustainable measures.
It is anticipated that primary care practices, through the IBH model, will be able to 1) provide on-site treatment for twenty to thirty percent of the patient population that is seen each year in the primary care practice (PCP) setting; 2) utilize behavioral health compacts for no more than twenty percent (20%) of patients that have moderate to high screening scores for depression, anxiety and/or SUD’s.
3-year pilot program with 2 waves of practices
- IBH Cohort I - Feb 2016 –December 2017
- IBH Cohort II - November 2016-October 2018
Cohort 1 |
Associates in Primary Care* |
| East Bay Community Action Program (E. Providence & Newport) | |
| Providence Community Health Centers – Chafee | |
| Tri-County Community Action* | |
| Women’s Medicine Collaborative* | |
Cohort 2 |
Brown University – Governor Street |
| Coastal Medical – Hillside Family Medicine | |
| Providence Community Health Centers – Capitol Hill | |
| Providence Community Health Centers – Prairie Avenue | |
| Wood River Health Services |
*Participated in the Major Depressive Disorder Learning Collaborative
Key Program Components:
- Support culture change, workflows, billing
- UniverOnsite IBH Practice Facilitation: sal Screening: depression, anxiety, substance use disorder
- Embedded IBH Clinician : warm hand offs, pre-visit planning, huddles
- Three PDSA Cycles : screening, high ED, chronic conditions
- Quarterly Best Practice Sharing: data driven improvement, content experts
Practice Payment: $35,000 over 2 Years
| Infrastructure Payment | 1st payment: month 1 | 2nd payment: month 5 |
| $15,000 prorated per 5000 attributed lives | $10,000 | $5,000 |
| Incentive Payment | Year 1: month 12 | Year 2: month 24 |
| $10,000 each year for meeting screening targets | Depression: 70% Anxiety: 50% Substance Use Disorder: 50% |
Depression: 90% Anxiety: 70% Substance Use Disorder: 70% |
Lessons Learned
CTC conducted a qualitative research evaluation study which included interviews with the practice staff and key stakeholders with the following barriers and recommendations identified:
- Co-pays are a barrier to treatment particularly when patients obtain “same day” care from IBH and Medical provider and when patients have to pay a higher specialist behavioral health co-pay;
- Billing and coding for behavioral health in primary care is difficult to navigate; practices recommended proving them with 6 months “startup” time to prepare for implementation; Recommendations made to consider an alternative payment system for IBH in primary care; Recommend obtaining up-front commitment from systems of care to provide practices with infrastructure support (i.e. EHR, Billing and Coding, recruiting and credentialing behavioral health clinicians);
- There is a need to build the integrated behavioral health workforce;
- Onsite practice facilitation by IBH subject matter experts supports culture change for successful implementation;
- There is a need to address the needs of smaller practices who have patients with behavioral health needs who may not have the capacity to hire on site behavioral health clinicians.
The full qualitative report can be found here and the executive report here and presentation here.
Results
Providers love it: “When I say how much I love having integrated behavioral health, it is that I can’t imagine primary care without it. It just makes so much sense to me to have those resources all in the same place because it is so important.” Provider indicated in the qualitative research study
Value of deliberate screening: “I’m surprised especially with the anxiety screener that there’s more out there than I knew about. I was talking to somebody yesterday. I know the patient pretty well, and the patients, if they had an issue, would tell me. But it comes up in a screener”. Provider indicated in the qualitative research study
Impact on ED use: “One of the things we identified through the program was somebody was going to the ER almost every other day and it was due to anxiety. So, he was giving tools to control that and it actually empowered him. He felt like he had taken control of the issue. And his ER visits dropped right off. He was being seen here (at the primary care practice) more frequently, but that’s OK. We’d rather he come here than go to the ER”. Practice Manager indicated in the qualitative research study
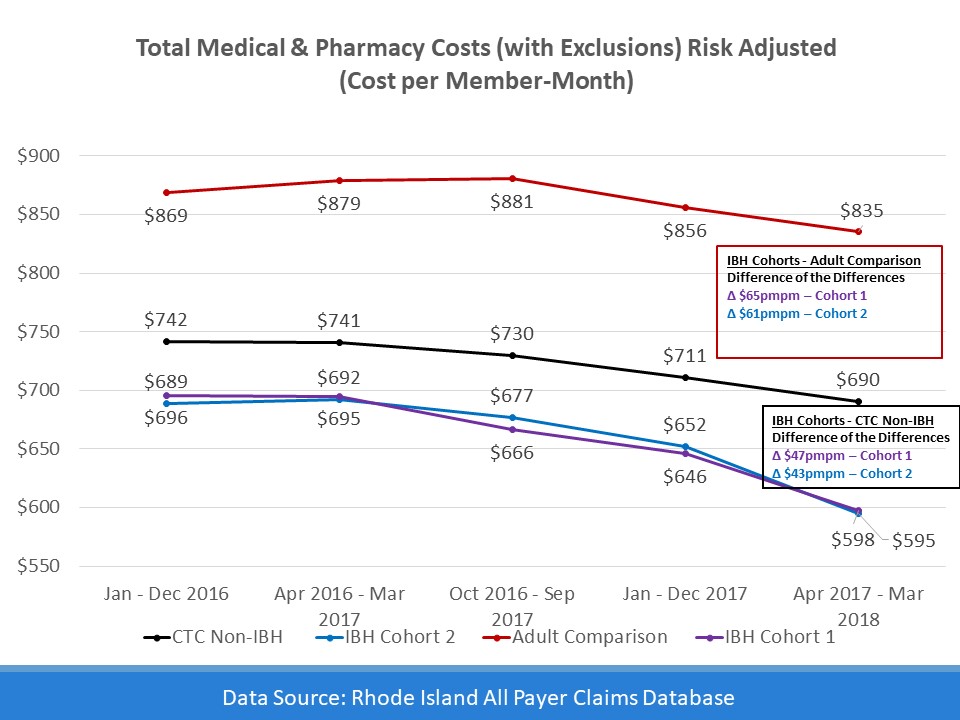
Total cost of care data from the All Payer Claims Database show significantly lower cost of care in practices that have integrated behavioral health program than the comparison groups. A more robust quantitative analysis from Brown University was also conducted and confirmed the positive effects of IBH intervention.

Our Mission
The mission of CTC-RI is to support the continuing transformation of primary care in Rhode Island as the foundation of an ever-improving integrated, accessible, affordable, and equitable health care system. CTC-RI brings together critical stakeholders to implement, evaluate and spread effective multi-payer models to deliver, pay for and sustain high-quality, comprehensive, accountable primary care.
