A Joint Message from Debra Hurwitz, RN, MBA and Pano Yeracaris, MD, MPH
A Small Project with a Big Impact––and Challenges Still to Come
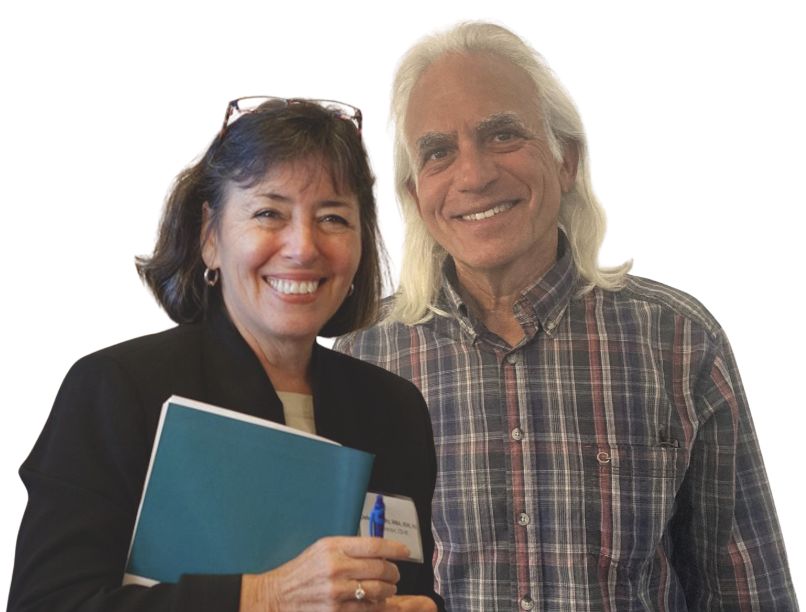
Pano Yeracaris, MD, MPH
The Chronic Care Sustainability Initiative (CSI) was launched in 2008 in response to a growing crisis in primary care. A statewide Patient-Centered Medical Home (PCMH) initiative––co-convened by the Office of the Health Insurance Commissioner and Executive Office of Health and Human Services/Medicaid––CSI brought together stakeholders to improve care delivery and coordination. Many individuals played a role in making that concept a reality. Debra became co-director in late 2011, and Pano joined as co-director in January 2014. Alongside Susanne Campbell, and later joined by Nelly Burdette, Linda Cabral, and many other dedicated partners, we helped grow what would become the Care Transformation Collaborative of Rhode Island (CTC-RI) into a strong, credible, and effective force for change.
In the spring of 2015, CSI transitioned into CTC-RI, a 501(c)(3) public-private partnership. That moment marked a new chapter, with Debra stepping into the role of Executive Director and Pano as Chief Clinical Strategist. For both of us, our work in Rhode Island has been the capstone of our careers––46 years for Deb and 44 years for Pano.
CTC-RI built on a proven model of quality improvement learning collaboratives, including practice facilitation, clear deliverables, and the integration of ECHO® learning. Our partnerships expanded beyond health plans and practices to include the Rhode Island Department of Health, Department of Behavioral Healthcare, Developmental Disabilities and Hospitals, and other collaborators and funders.
A defining principle of our work was the full embrace of team-based care. Nurse Care Managers, Medical Assistants, Integrated Behavioral Health (IBH) clinicians, pharmacists, and Community Health Workers became essential members of the care team. Together with clinical and community partners, we helped establish regional Community Health Teams––a model rooted in continuous improvement and real-world success. While this model was unfortunately phased out in 2021 for various reasons, its lessons remain valuable.
Today, we face a renewed crisis in primary care, driven by chronic underinvestment and the shifting of financial risk beyond the control of primary care practices, such as rising pharmaceutical costs. The May 2021 NASEM report affirmed the essential role and value of high-quality primary care and its designation as a “public good.” Its findings echoed CTC-RI’s April 2021 report on Comprehensive Primary Care Capitation, developed in response to COVID. Together, these reports offered a playbook for advancing primary care. But despite this clear guidance, multi-payer sustainable payment for team-based care has yet to take hold––and the underfunding of primary care continues.
In the aftermath of COVID, the crisis in our primary care workforce became even more visible. Early retirements, practice closures, and the departure of providers from Rhode Island accelerated a workforce shortage that was already underway. At the request of our CTC-RI Board, we convened a workforce task force co-chaired by Jeff Borkan and Denise Coppa. This group brought together program directors from all of Rhode Island’s primary care training programs for physicians, nurse practitioners, and physician assistants. The result was a comprehensive roadmap featuring six strategic goals and actionable recommendations. We’re pleased to see early progress, including new legislation aimed at compensating primary care practices for expanding preceptor capacity and standardizing training in the advanced primary care model.
As we transition to the next chapters of our lives, we are filled with gratitude. We are proud of the work we’ve accomplished together and of the incredible CTC-RI team––project coordinators, project managers, and leaders alike. We pass the torch with full confidence that CTC-RI will help Rhode Island meet the challenges ahead. We call on our many partners and stakeholders to continue pushing this work forward.
We have collectively answered questions on “what to do” and “how to do it.” Now, we must urgently address “how to pay for it”––in a way that is both sustainable and impactful. This will require a realistic understanding of costs (as reflected in the literature and tools like the Practice Cost Calculator), and a clear articulation of expectations and responsibilities––on quality, access, patient experience, cost containment with specialists and hospitals, and meaningful engagement with community-based organizations.
 We also urge the revitalization of the regional Community Health Team model, with Community Health Workers and Behavioral Health clinicians playing key roles in addressing health-related social needs and bridging the gap between primary care, Certified Community Behavioral Health Clinics, and other community organizations.
We also urge the revitalization of the regional Community Health Team model, with Community Health Workers and Behavioral Health clinicians playing key roles in addressing health-related social needs and bridging the gap between primary care, Certified Community Behavioral Health Clinics, and other community organizations.
Rhode Island must be bold. It’s time to take the next step––to make meaningful investments in team-based care and to create strong, coordinated incentives that foster collaboration across the healthcare system.
We wish you all continued success—and offer our deepest thanks for the opportunity to be part of this journey.
Deb and Pano
